Understanding and Controlling Gestational Diabetes
Gestational Diabetes: Managing Blood Sugar During Pregnancy
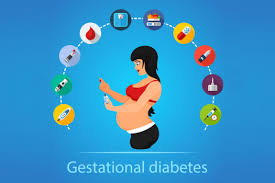
Gestational diabetes is a form of diabetes that develops during pregnancy, usually in the second or third trimester. It occurs when the body cannot produce enough insulin to meet the increased needs of pregnancy, leading to high blood sugar levels. Proper management through diet, exercise, and sometimes medication is crucial to protect both mother and baby.
Gestational Diabetes: Causes, Management, and Health Implications
Gestational diabetes is a temporary form of diabetes that occurs during pregnancy, affecting how the body processes glucose. It usually develops in the second or third trimester when the body’s insulin needs increase, and hormonal changes interfere with insulin function. While the exact cause isn’t entirely understood, risk factors include being overweight, having a family history of diabetes, and being older than 25 when pregnant. Gestational diabetes doesn’t usually cause noticeable symptoms, but it can increase the risk of complications such as high birth weight, preterm birth, and the need for a cesarean section. Regular screening during pregnancy helps in early detection and management.
Managing gestational diabetes focuses on keeping blood sugar levels within a healthy range to ensure a safe pregnancy and delivery. A balanced diet rich in whole grains, vegetables, lean proteins, and healthy fats helps manage blood sugar levels. Carbohydrate counting and portion control are key strategies, as they help balance insulin needs and glucose intake. Regular physical activity, such as walking or prenatal exercise classes, improves insulin sensitivity and helps keep blood sugar levels stable. Monitoring blood glucose levels regularly, often several times a day, is crucial to understanding how food and activity affect blood sugar.
If lifestyle changes alone are not sufficient to control blood sugar, medication such as insulin or oral glucose-lowering drugs may be prescribed. It’s important to work closely with healthcare providers, including obstetricians, dietitians, and diabetes educators, to develop a personalized management plan. Maintaining control over blood sugar levels during pregnancy helps reduce the risk of complications and contributes to a healthy pregnancy outcome. Women who have had gestational diabetes are at an increased risk of developing type 2 diabetes later in life, so continued monitoring and healthy lifestyle choices are essential after pregnancy.
Support from healthcare professionals and family is vital for women managing gestational diabetes, as it can be challenging and emotionally taxing. After delivery, blood sugar levels usually return to normal, but the experience of gestational diabetes can serve as a wake-up call to prioritize long-term health. Postpartum follow-up and regular screening for type 2 diabetes are recommended. Preventive measures such as maintaining a healthy diet, staying active, and achieving a healthy weight can help reduce future diabetes risk. Understanding and managing gestational diabetes not only supports a healthy pregnancy but also sets the foundation for better health in the years to come.