Understanding the Key Differences
Type 1 vs. Type 2 Diabetes
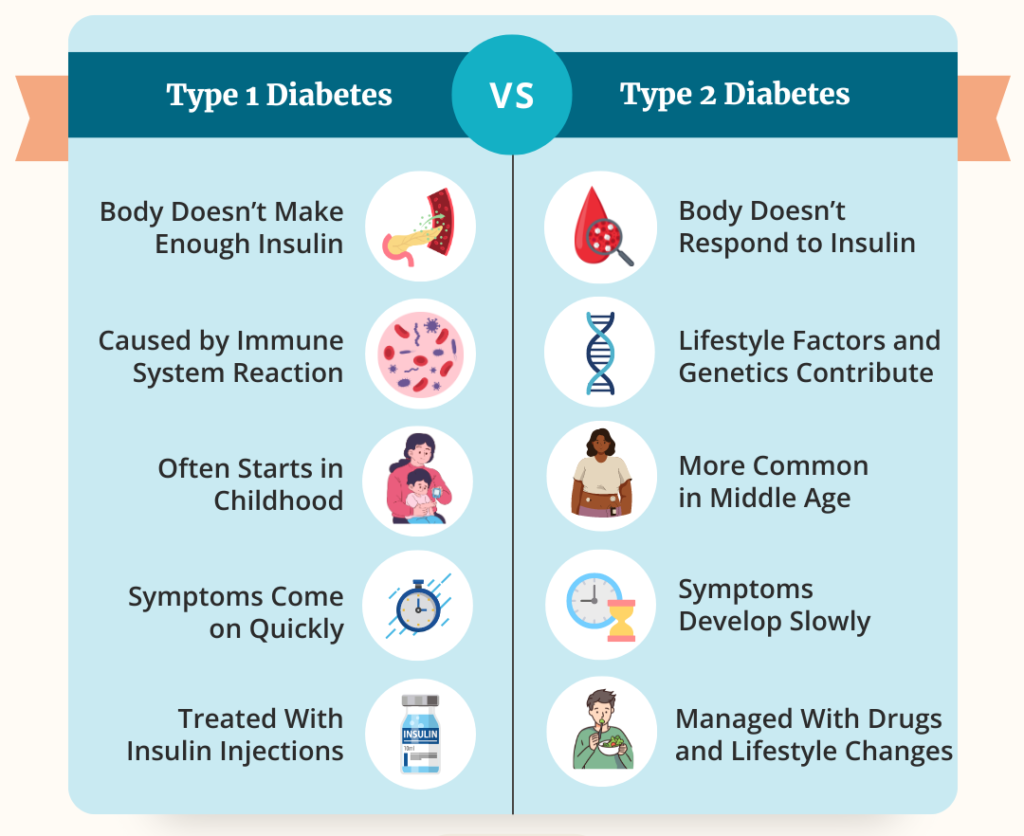
Learn the important differences between Type 1 and Type 2 diabetes. This section breaks down how each type affects the body, their causes, and common treatment approaches. The image on the right provides a clear comparison to help you understand these two distinct forms of diabetes.
What is type 1 diabetes?
Type 1 diabetes is a chronic condition where the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the body is unable to produce insulin, a hormone that helps regulate blood sugar levels by allowing glucose to enter cells for energy. This lack of insulin leads to high blood sugar levels, which can cause various complications if not managed properly. Type 1 diabetes often develops in children, teenagers, or young adults, but it can occur at any age.
Managing Type 1 diabetes requires lifelong insulin therapy, either through injections or an insulin pump, along with careful monitoring of blood sugar levels, a healthy diet, and regular physical activity. While the exact cause of Type 1 diabetes is unknown, it’s believed to involve a combination of genetic and environmental factors. Unlike Type 2 diabetes, lifestyle factors like diet and exercise do not cause Type 1 diabetes, making early diagnosis and consistent management crucial to maintaining health and preventing complications.
What is type 2 diabetes?
Type 2 diabetes is a chronic condition where the body becomes resistant to insulin or doesn’t produce enough insulin to maintain normal blood sugar levels. This leads to elevated glucose levels in the bloodstream, which, over time, can cause serious health complications such as heart disease, kidney damage, and nerve issues. Type 2 diabetes is the most common form of diabetes, primarily affecting adults, although it’s increasingly seen in younger individuals due to rising obesity rates and sedentary lifestyles.
Unlike Type 1 diabetes, Type 2 is often linked to lifestyle factors such as poor diet, lack of physical activity, and excess weight, particularly around the abdomen. Management of Type 2 diabetes focuses on lifestyle changes, including a balanced diet, regular exercise, and weight loss, which can significantly improve blood sugar control. In some cases, medications or insulin therapy may be necessary to help manage the condition. Early detection and proactive management are crucial to preventing the long-term effects of Type 2 diabetes.